Trust

From those first overwhelming moments when we learn that we have a serious illness, we begin to learn.
By Christine Wilson
Project Innovation brought together a group of patients and caregivers to talk about what it means to make shared decisions and to advocate effectively for themselves and their larger communities. All 15 of these individuals are facing cancer, most of them for many years. The group included long-term survivors of advanced lung, breast, appendix, prostate and colon cancer, caregivers and people who carry genetic mutations that significantly increase their likelihood of getting cancer. They came from all over the country, men and women of different ages and life experience. In this facilitated Zoom meeting, they spoke openly to each other about their relationships with their doctors, their values and priorities and the need for good information and navigation to help them make shared decisions about their treatment and care.
I started my career many years ago with the NCI funded program, Cancer Information Service. I was young and had no real experience with serious illness, just a library of materials on various cancers and resources available to patients.
Every day, I answered calls from people facing cancer. We didn’t give medical advice but we did try to help people understand their condition and its treatment. The calls were about every kind of cancer, from the most common to the rarest, from patients and caregivers, young and old. Some people were terrified, others angry, others determined and focused on finding the best treatment for themselves or others. I could take a call from a person with all the medical studies printed and lined up in front of her, and the next one would be from a newly diagnosed patient who did not understand the tumor and cancer were the same.
I learned a lot from this experience. It’s not just a cliche when we say that everyone has a unique and powerful story. Since my Cancer Information Service days, I have interviewed thousands of patients and been struck over and over again by the insight and individual perspective that each one of these people bring to their experience.
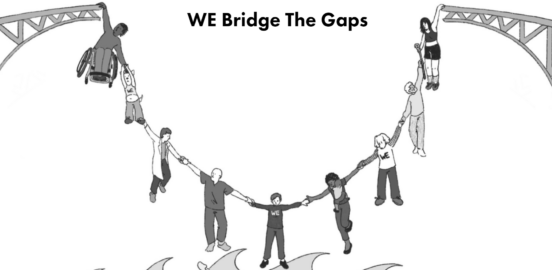
It’s also remarkable how much patients and caregivers learn as they move through their illness journey. We may all begin as “strangers in a strange land,” unable to speak the language or understand the customs of this frightening new world into which we have been thrown. But, from those first overwhelming moments when we learn that we have a serious illness, we begin to learn: how to find information, what questions to ask, and how to ask them, what resources are available to help us and which ones are not there. We get better at working with our Byzantine, often impersonal health care system. We become our own best advocates, and sometimes grow to use our skills to advocate for our communities and for meaningful change.
People who have lived with cancer, especially advanced forms of cancer, all have long, difficult stories to tell. There is real progress but it comes with a price. If you have survived for multiple years with advanced lung cancer, stage IV breast cancer or a rare tumor such as appendix cancers, you know what it means to make a shared decision with your doctor. You understand the importance of having a trusting relationship with that doctor, but also of having someone you trust, a navigator or peer, to help find your way through the decision making processes, to find your way through the system, to put you into contact with other people who share parts of your experience. Many people living with advanced care recognize the enormous impact of new treatments that bring longer life, along with more challenges at every level, medical, social and financial. Patients and caregivers come to understand the importance of defining what is important to you, at that point in time, and bringing those values and priorities to the decision making process.
The only way to gain access to the insight, wisdom and knowledge that patients and caregivers have and can articulate is to….listen. That means providing people with the opportunity to share their experiences and tell their stories, to respect them and even more important to incorporate those patient voices into every step of the treatment and care decision making process. It was a privilege to listen when I answered those Cancer Information Service calls all those years ago, and it remains even more so today.
Participants
Amelia: Breast cancer patient since 2019, under treatment
Anita: 17 year colon cancer survivor
Florence: 22 year stage III colon cancer survivor
Gary: Stage IV appendix cancer, under treatment
Heather: Four year Stage III colon cancer survivor
Julie: Three time cancer survivor
Kimberly: Caregiver for husband and mother
Sunshine: Stage IV breast cancer
Marquita: Breast Cancer with interest in young women diagnosed with breast cancer
Larry: Nine year Stage IV lung cancer survivor
Mike: Eight year prostate cancer survivor, BRCA2 mutation
Sally: Lung cancer survivor with three generations of lung cancer in her family
Lynne: 21 year breast cancer survivor with recent recurrence
Tia: 10 year Stage IV breast cancer survivor
Verinda: BRCA1 carrier and caregiver for her sister who died of breast cancer
Yasmeen: Nine year Stage III colon cancer survivor
Highlights
“It’s [shared decision-making] a key issue for those of us who have been on treatment for a long time, for three, five or 10 years. It’s the ability to customize your treatment experience and do so in a perspective that is informed….I’d like to take control of the experience so that I can have a quality of life that’s sustainable over a long time.” -Amelia
“I have appendix cancer, and it’s been a pretty rough ride. And, I’ve been thinking a lot at this point, what are my options…..Wouldn’t it be great if I had a cancer coach, who knew all the options and could outline the decision tree and point to this path if you want to accomplish this or that one if you want this to happen.” -Gary
“In my nine years of treatment for stage IV lung cancer, shared decision making points have occured when there was progression and I needed to do something different….I think the most comforting thing I have heard from my oncologists at those points is that there’s no wrong answer…They have given me some good options and I have tended to favor decisions that in alignment with my quality of life.” -Larry
“This is not something we can do alone. And we have to be advocates for other people. I have no trouble speaking up for myself but there are so many others that are not like that. And when you are not a person who is your own advocate, you tend to get lost in the shuttle.” -Lynne
“The doctor looked at me and said, ‘the good news is that cancer is 100 percent treatable and I can go on that journey with you’…He told me everything that was going to go on and what would happen with my body, but he said, ‘everything is our choice, our plan together.” -Sunshine
“There aren’t a lot of stage IV people who live for five years, and they didn’t always know what to do with me. So, we did a lot of shared decision making. There wasn’t always a protocol so he [the oncologist] sort of had to make it up as went along, and we did it together.” -Anita
This is the first of a three part series. Part II will focus on Decision Support Tools and Part III on Navigation and Support.
Trust
Caregiving, Health Literacy, Needs Navigation, Trust
Caregiving, Storytelling, Trust
Equity, Health Literacy, Insurance, Policy Consortium