Caregiving

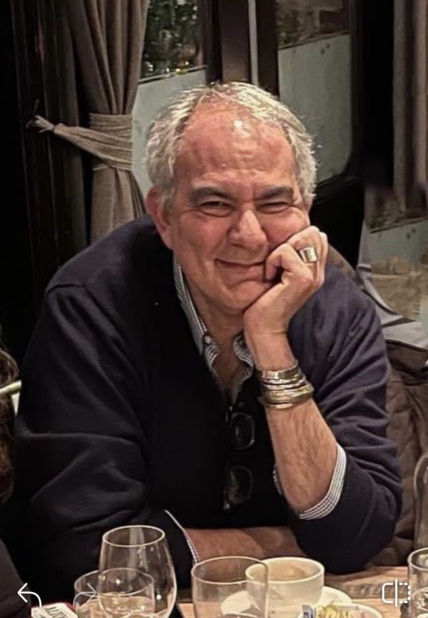
NPAF Advocate Bruce Weinstein shares his take on NPAF's listening session held October 15, 2024.
Bruce Weinstein recently joined NPAF’s grassroots network. He is a food writer and cookbook author with degree in Fine Arts. He is currently studying at CSU nursing school to become a board-certified patient advocate. He also volunteers at Yale New Haven Hospital and sits on the Smilow Cancer Center Patient Family Advisory Council. He lives in Connecticut with his husband (and business partner) with whom he has so far written and published 41 books.
During this past year, my husband was diagnosed with a potentially deadly pancreatic condition which was dismissed with the wave of a hand by the first GI doc we consulted. My husband felt abandoned by this man – the head of his department at a world-class university medical school hospital. I was angry. And it spurred me into researching a better care team that would listen to our concerns and put us on a path of scans and treatments that might just save my husband’s life. At the same time, my best friend was diagnosed with a recurrence of her 3rd cancer and was offered confusing and opposite opinions from different doctors in her care team, also at a world class university institution. Not sure what questions to ask nor to whom they should be addressed, she reached out to me knowing what I had done to help my husband. Overnight I became a patient advocate for them both.
They, like thousands of others who have gotten caught up in the complex medical system in the US, needed answers to questions they hadn’t even formulated yet and they needed the right support team to make an intolerable journey a little more human. I was honored to take on the task of helping them be heard.
This work was new to me and just felt right. And somehow easy. A strange word to use when describing navigating our industrial medical complex. But I saw what was working for us and what wasn’t. And I was there to help make things right. They had a voice.
Now I needed to be heard. And on October 15th I was heard at my first listening session as part of NPAF’s Policy Consortium. I had contacted the folks at NPAF a few weeks earlier for guidance and advice on this exciting but fraught road I was heading down. They asked if I would share my story along with other advocates as we tried to make medical care a little easier and accessible for everyone.
What I learned was that my best friend and my husband’s situations are not unique, and we are not alone on this quest to be heard over the chaos that exists in today’s healthcare system,
But being heard is just one of five important issues that struck me while listening to others talk at the symposium about their experiences as patients, advocates, and policy makers.
Being educated was the just as important as being heard. What surprised me though, was the idea that education wasn’t just limited to the patient experience, learning about your disease and how to treat it. Advocates need to be educated as well as physicians, hospital administrators, and yes, even insurance companies. We all need to be educated about what patients really need alongside their treatment. Because if we fall short there, everyone suffers, and the system will fail for all of us.
I learned what education looked from Leslie Bennet when she talked about how the high cost of meds can lead providers and insurers to limit their use even while the potential healthcare savings they can bring in the long run can far outweigh their upfront cost. I learned from Erika Olinsky that the trauma induced by a journey through the US healthcare system isn’t just limited to the patient. But also the family and everyone who has contact with them.
The cost of healthcare was a common theme from all the speakers at this symposium. I learned how even the fear of high costs can impact the accessibility of treatment and outcome of disease. I learned from Martha Sanchez that even young adults are plagued by diseases we associate with older folks and how important it is having affordable insurance plans through the ACA for everyone.
Another revelatory moment for me was learning that every patient’s support-needs is as idiosyncratic as their treatment. Patient support and patient advocacy is not a one-size-fits-all situation. As Heidi Kummer – president of the Patient Advocate Certification Board said – it is the interpersonal connections that will make change. Understanding what each individual patient and their family needs is the only way to navigate successfully through our fractured healthcare system.
Advocacy is done on the patient level, the community level, and on the policy level. And clearly listening to each other and communicating through all levels is the only way serious changes will be made to help make this work for all of us.
We all talked about our desire for a more transparent system. One that clearly communicates every step in patient care from the tech required to make appointments to what the narrative arc of care and recovery looks like in each patient’s case. I learned that transparency is not just better communication between doctors and patients nor between patients and their families and advocates. But between all of us trying to make changes in the system. Between patients, private advocates, public advocates, hospital administrators, health care providers, and policy makers. Advocacy is done on the patient level, the community level, and on the policy level. And clearly listening to each other and communicating through all levels is the only way serious changes will be made to help make this work for all of us.