
Shared Decision Making for People with Cancer and Other Serious Illness
The value of patients collaborating with healthcare professionals in the face of long-term illness.
Overview
The Long Illness Journey
Health-care advances mean that many people with cancer are living much longer. Patients with cancers that once led to death in weeks or months can now survive for years; that doesn’t mean they’re cured—they’re still being treated for their disease. And as a result, patients and caregivers need to make more decisions about their treatment, their care, and their lives.
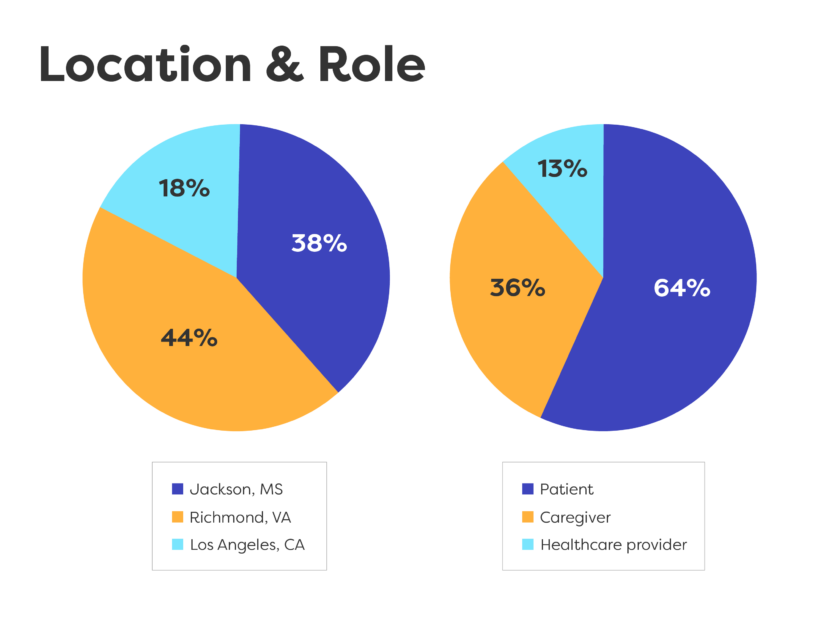
We worked with three community partners to learn more about what shared decision making means to people living with cancer and other serious diseases, asking critical questions:
- How do they become true partners in their care?
- What barriers exist to accessing these remarkable new treatments?
- How do they talk to doctors and health care providers about difficult issues?
“The future of cancer treatment is here, but today, it’s benefits are not evenly distributed”
—Robert Winn, MD
Keynote Address
NPAF Policy Consortium, Fall 2023
Policy Consortium Fall 2023
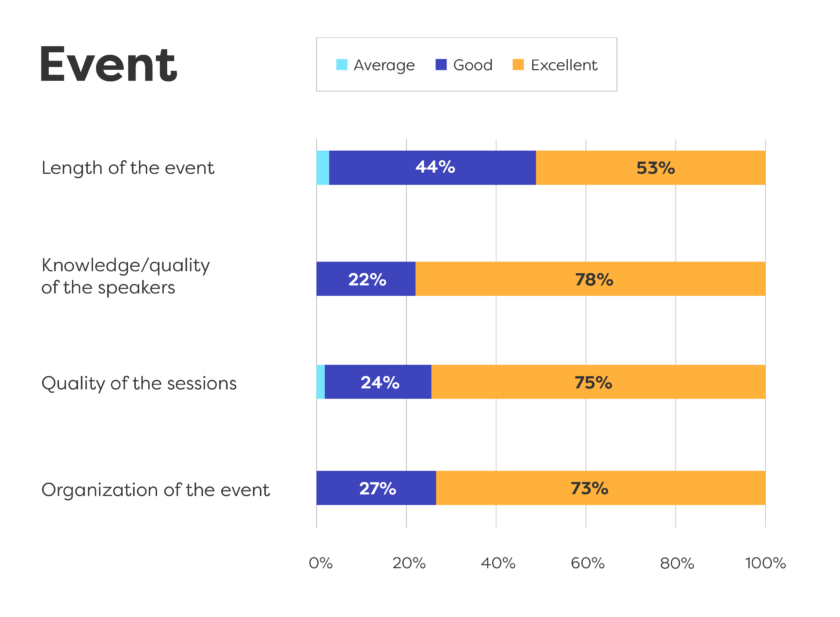
In November, NPAF held its Fall Policy Consortium to review the project’s work to date; to hear the voices of patients, caregivers and health care providers; and to present recommendations so people can make shared decisions and get the best care.
We thank the Danaher Foundation for their support through Project Innovation.
Community partners:
- Freddie White Johnson
Fannie Lou Hamer Cancer Foundation
Ruleville, Mississippi - Robert Winn, MD
Massey Comprehensive Cancer Center
Virginia Commonwealth University
Richmond, Virginia - Viviana Criado
Los Angeles Alliance for Community Health and Aging
Los Angeles, California
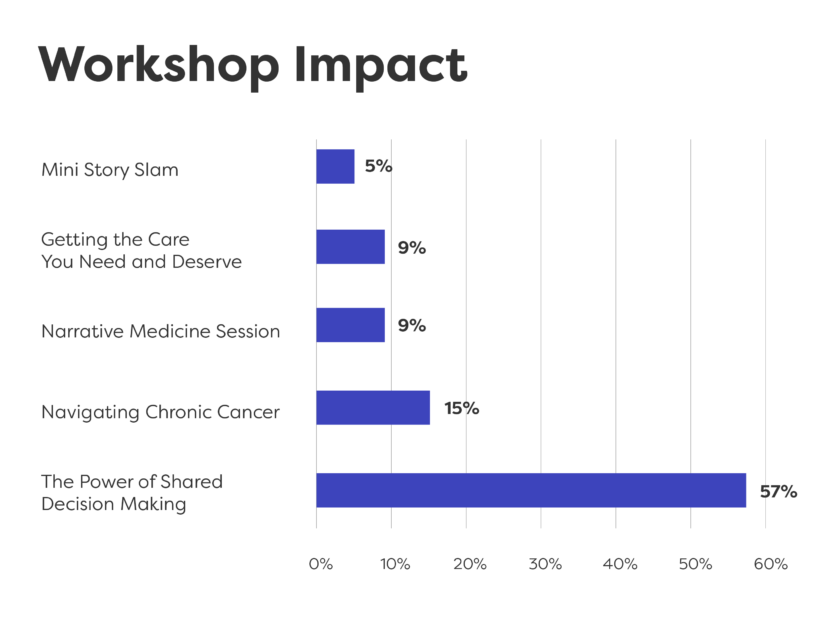
Our workshops were:
- Co-created
- Highly interactive
- Involved discussion with patients and health care providers
- Presented opportunities for patients and caregivers to tell their stories, to be heard and to listen to others
Key Learnings

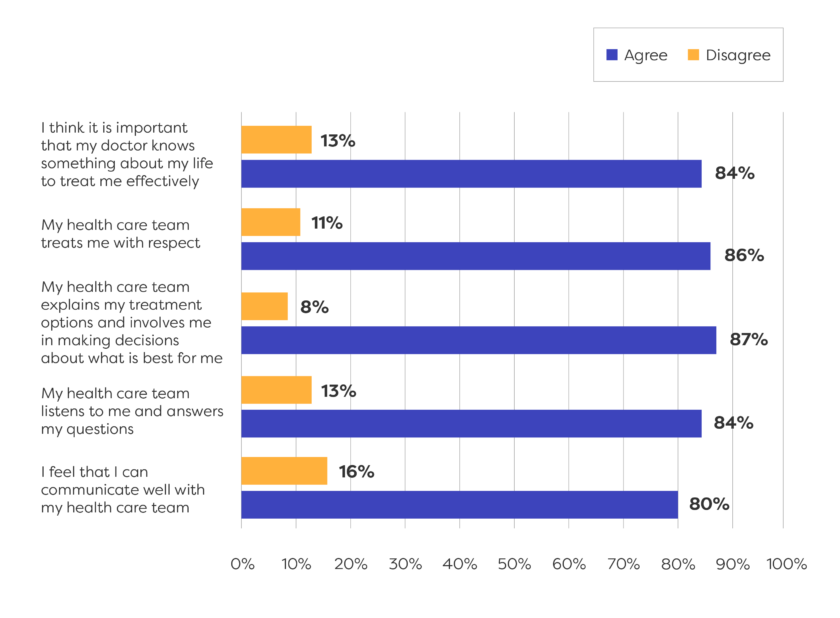
Shared Decision making depends on mutual trust between patients and their provider.
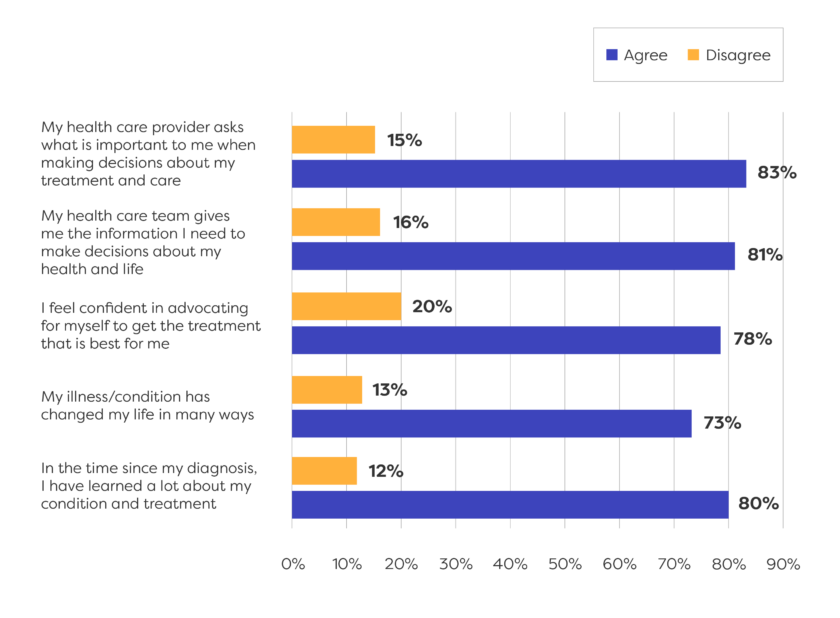
Patients want relationships with providers who know them and understand their priorities.
Patients want information about their treatment and care options up front—before their appointments—so they can ask the right questions.
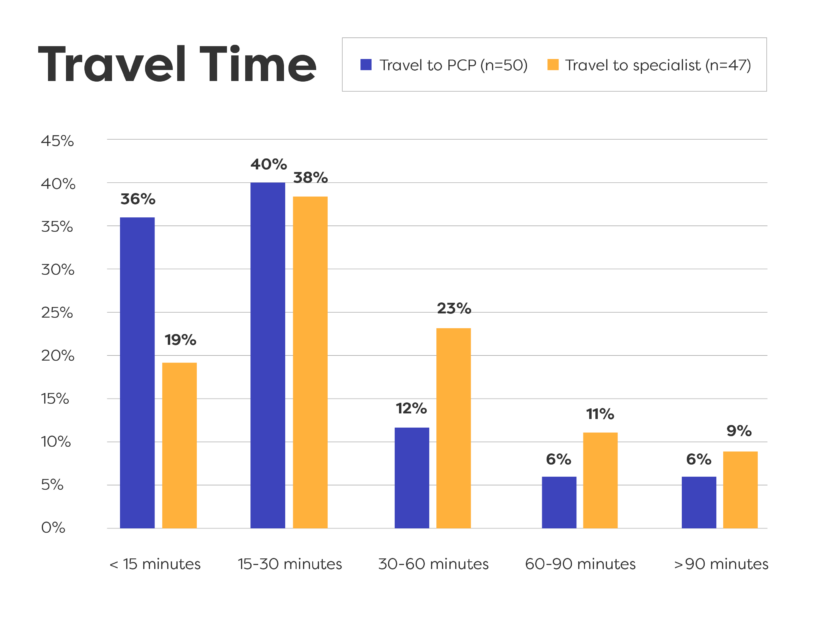
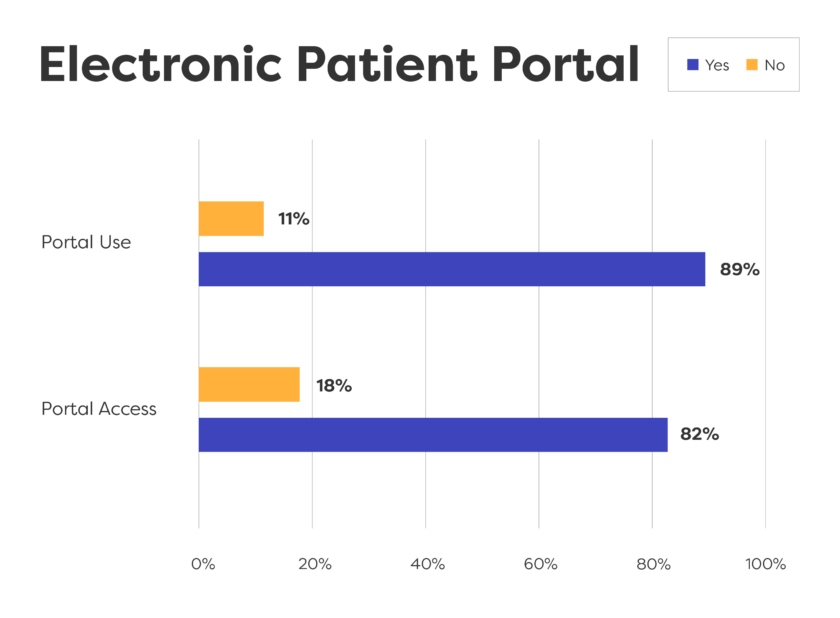
Many patients can use electronic patient portals and phones to get information, but rural areas often lack good wifi.
People become better advocates for themselves and are better able to navigate the healthcare system as they move through their illness journeys.
Many patients want to take what they've learned from their experience to help others facing serious illness.
Difficult Topics

Conversations or decisions that involve “bad news,” including changes in treatment or ending treatment.
Fear of being judged because of who they are or something they’ve done.
Talking about the costs of care or insurance status.
Gaining understanding and acceptance from family members about difficult decisions.
From the Blog
Next Steps

The Fight for Health Equity
The future of cancer treatment is here—the benefits just aren’t equally distributed.


